About one in three patients would be reclassified to more severe chronic kidney disease stage
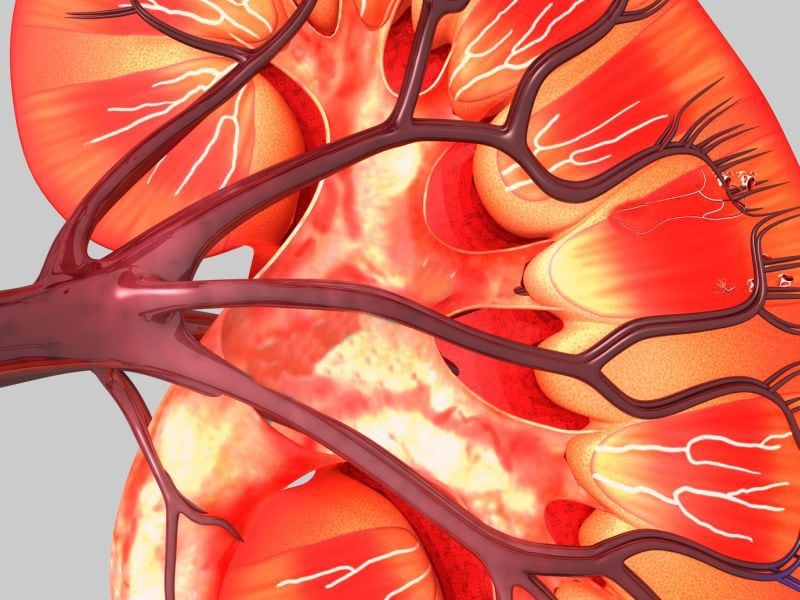
TUESDAY, Oct. 20, 2020 (HealthDay News) — About one in three African American patients with chronic kidney disease (CKD) would be reclassified to a more severe CKD stage if the race classifier were removed from the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation, according to a study published online Oct. 15 in the Journal of General Internal Medicine.
Salman Ahmed, M.D., M.P.H., from Brigham and Women’s Hospital in Boston, and colleagues examined the impact of the race multiplier for African Americans in the CKD-EPI estimated glomerular filtration rate (eGFR) equation on CKD classification and care delivery. Data were included for 2,225 African American patients in the Partners HealthCare System CKD Registry.
The researchers found that if the race multiplier were removed from the CKD-EPI equation, 33.4 percent of the African American patients would hypothetically be reclassified to a more severe CKD stage; 24.3 percent would be reclassified from stage 3B to stage 4 and 3.1 percent would be reassigned from eGFR >20 to ≤20 mL/min/1.73 m², meeting the criterion for accumulating kidney transplant priority. After the race multiplier was removed, 64 patients were reclassified from eGFR >20 to ≤20 mL/min/1.73 m²; none of these patients were referred, evaluated, or waitlisted for kidney transplant compared with 19.2 percent of African American patients with eGFR ≤20 mL/min/1.73 m² using the default CKD-EPI equation.
“Considering the inequities in kidney care and outcomes for Black patients, use of the eGFR race correction factor needs to be reconsidered,” a coauthor said in a statement.
One author disclosed financial ties to the pharmaceutical industry.
Abstract/Full Text (subscription or payment may be required)
Copyright © 2020 HealthDay. All rights reserved.